Projects
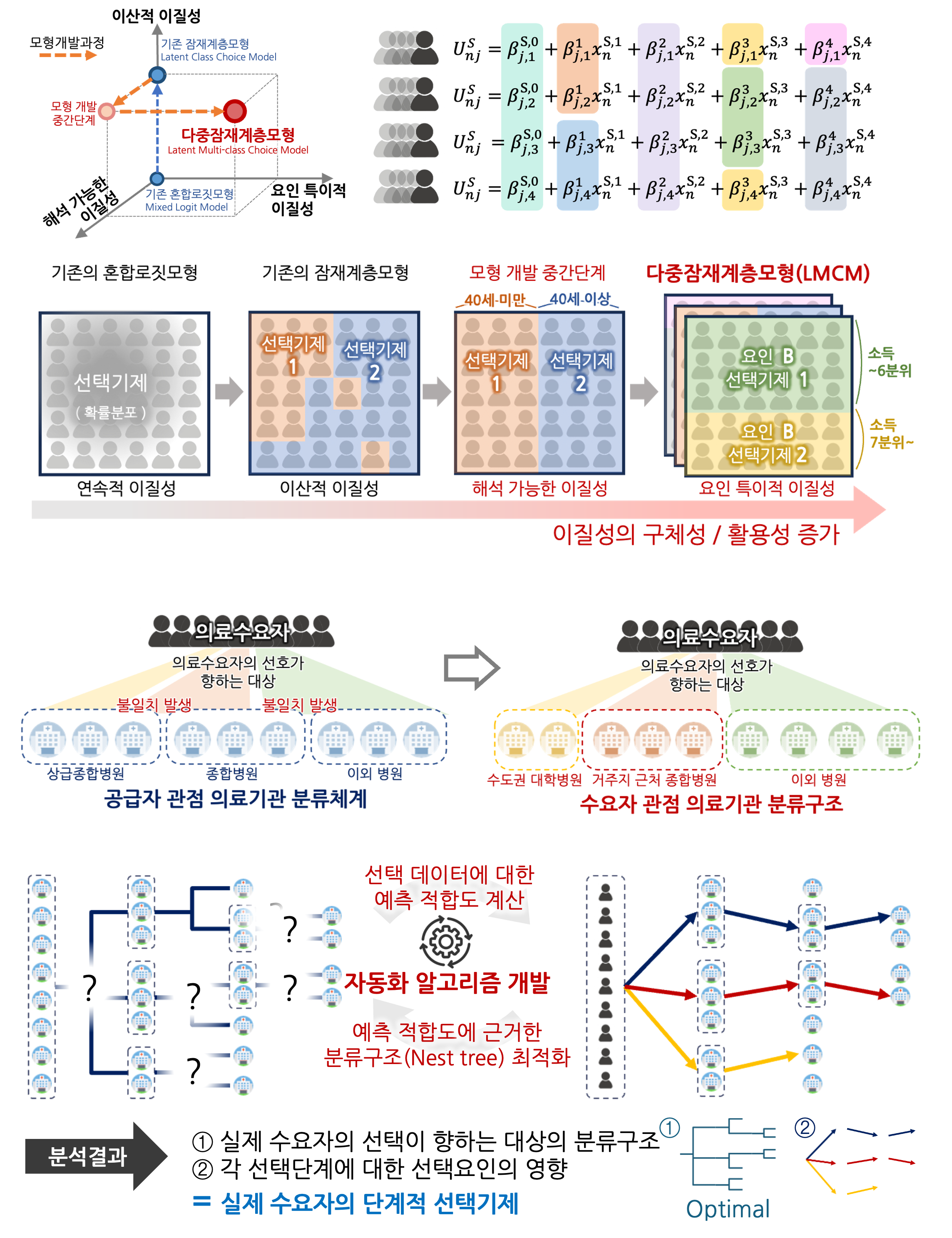
Advanced Discrete Choice Model for Hospital Preference Analysis
In the Korean healthcare system, patients are afforded a high level of autonomy in choosing hospitals, a privilege that paradoxically contributes to systemic inefficiencies and potentially inadequate utilization of services. A comprehensive understanding of these decision-making processes is crucial to enhance the operational efficiency of the national healthcare system. This research focuses on elucidating patient hospital choice behaviors using the Discrete Choice Model (DCM), which interprets the influence of various factors within the framework of human decision-making theories. The objective is to refine and adapt DCM structures in two distinct ways while concurrently developing corresponding estimation algorithms. The introduction of a Latent Multi-class Choice Model (LMCM) aims to capture the heterogeneity in utility functions, which may be influenced by contextual backgrounds and personal experiences. Given the constraints of existing models, the LMCM seeks to provide a more detailed and comprehensive characterization of choice heterogeneity. Additionally, this study utilizes the Nested Logit model to derive a nest structure from choice data, which facilitates the exploration of a hierarchical hospital structure from the perspective of the patients.
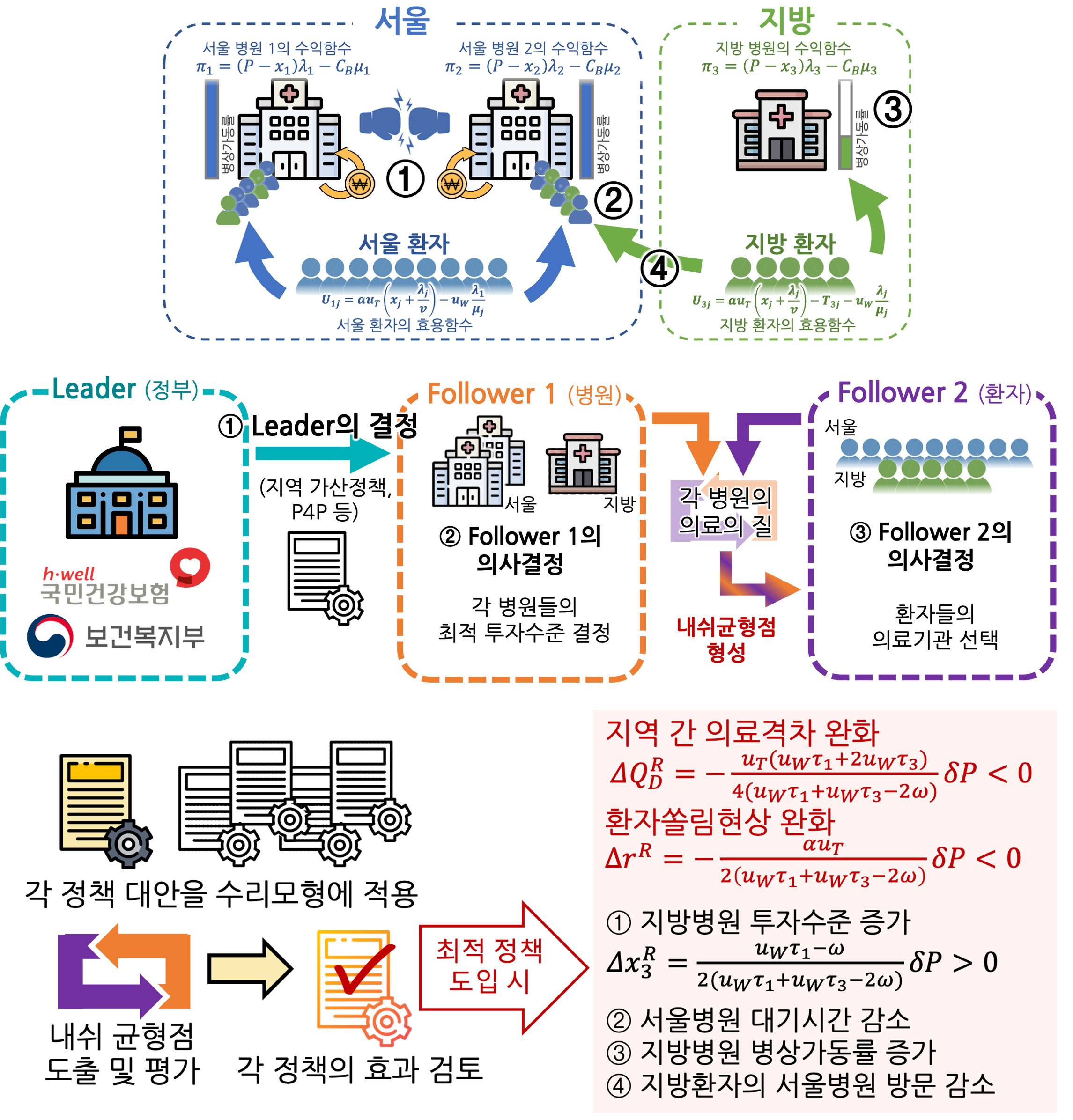
Healthcare Payment System Optimization
Our research aims to develop a game theory-based mathematical model to represent patient concentration at large hospitals in Seoul. The model will capture the dynamics of increased local competition driving inter-regional competition and patient influx. Additionally, it will incorporate the relationship between treatment volume and healthcare quality, reflecting the impact of treatment volume on outcomes. Using mathematical optimization and game theory, we will derive Nash equilibria to explore the effects and mechanisms of various policies based on these equilibria. This includes analyzing the impact of current policy discussions, such as penalties for using hospitals in other regions, direct investment in local hospitals, and increased medical fees for local hospitals. We will also propose new policies, such as expanding and strengthening pay-for-performance systems and providing operational support for local hospital expansions. Furthermore, the model will be extended to account for patients' risk-averse behavior by modifying their utility functions from risk-neutral to risk-averse, observing the changes in optimal government policies. This comprehensive approach aims to identify effective strategies to mitigate patient concentration at major hospitals and improve the overall healthcare system.
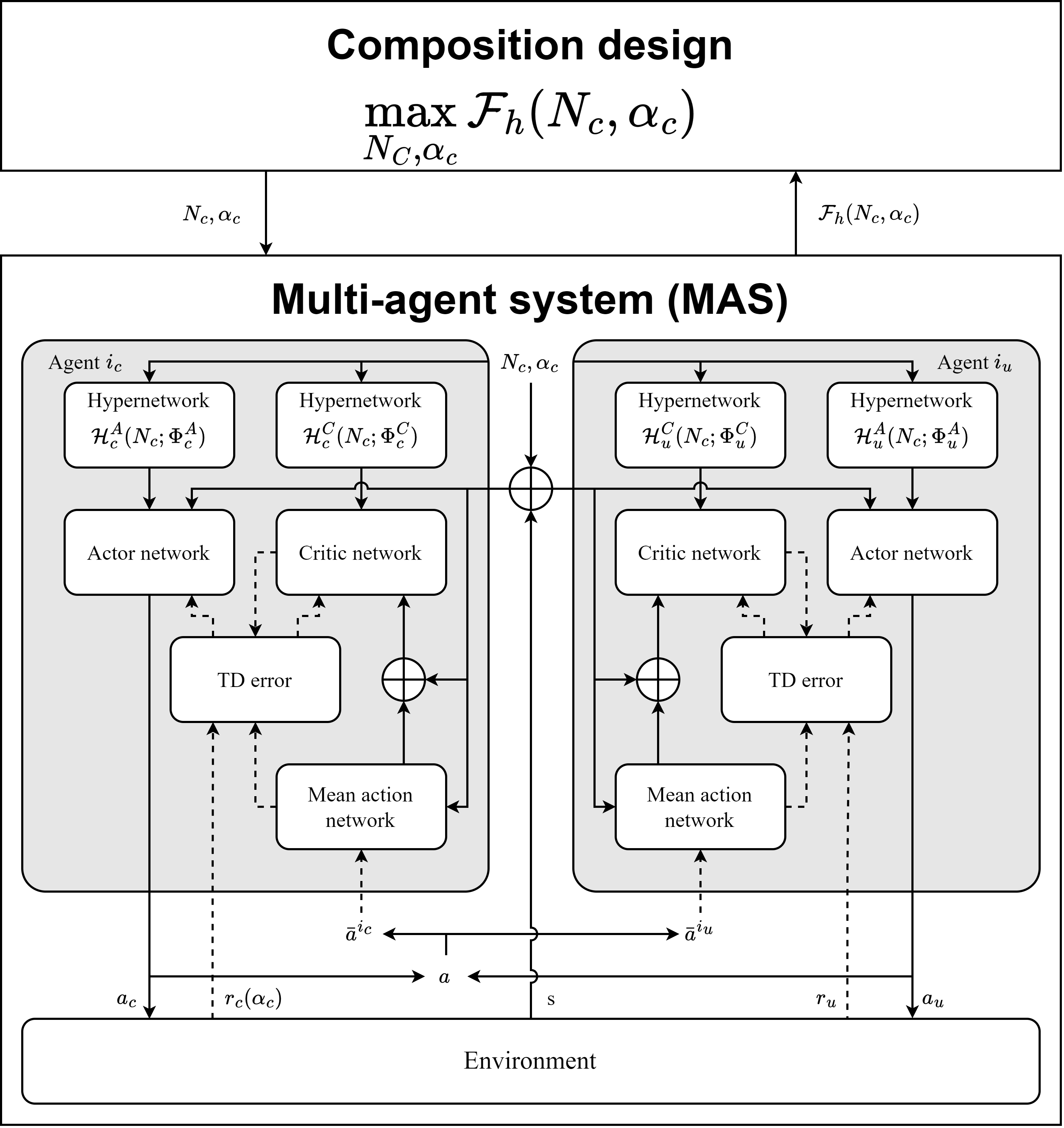
Optimization for Human-Autonomous Agent Collaboration Decision Making
In hybrid environments involving both manned and unmanned systems, complex design problems arise, such as determining the optimal functional and quantitative composition of autonomous agents and human agents to maximize overall system effectiveness. Additionally, designing the optimal policies for human agents in engagement scenarios dominated by autonomous agents presents significant challenges. To address these complexities, our research aims to develop optimized decision-making techniques for human-autonomous agent collaboration by leveraging bi-level optimization and multi-agent reinforcement learning with hypernetwork structuring. (Partially Controlled Multi-Agent Systems) Hybrid systems offer advantages over fully autonomous systems by integrating the flexibility and adaptability of human agent decision-making. Autonomous decision-making agents, equipped with policies learned through reinforcement learning, interact with human agents in a dynamic system environment. From the perspective of human agents, autonomous agents represent part of the system environment, and vice versa. Through these interactions, human agents can more efficiently guide the decision-making of autonomous agents towards system-wide optimal outcomes. This requires optimizing the functional and quantitative composition of agents in the hybrid environment and calculating the optimal policies for both human and autonomous agents to achieve the best system configuration.
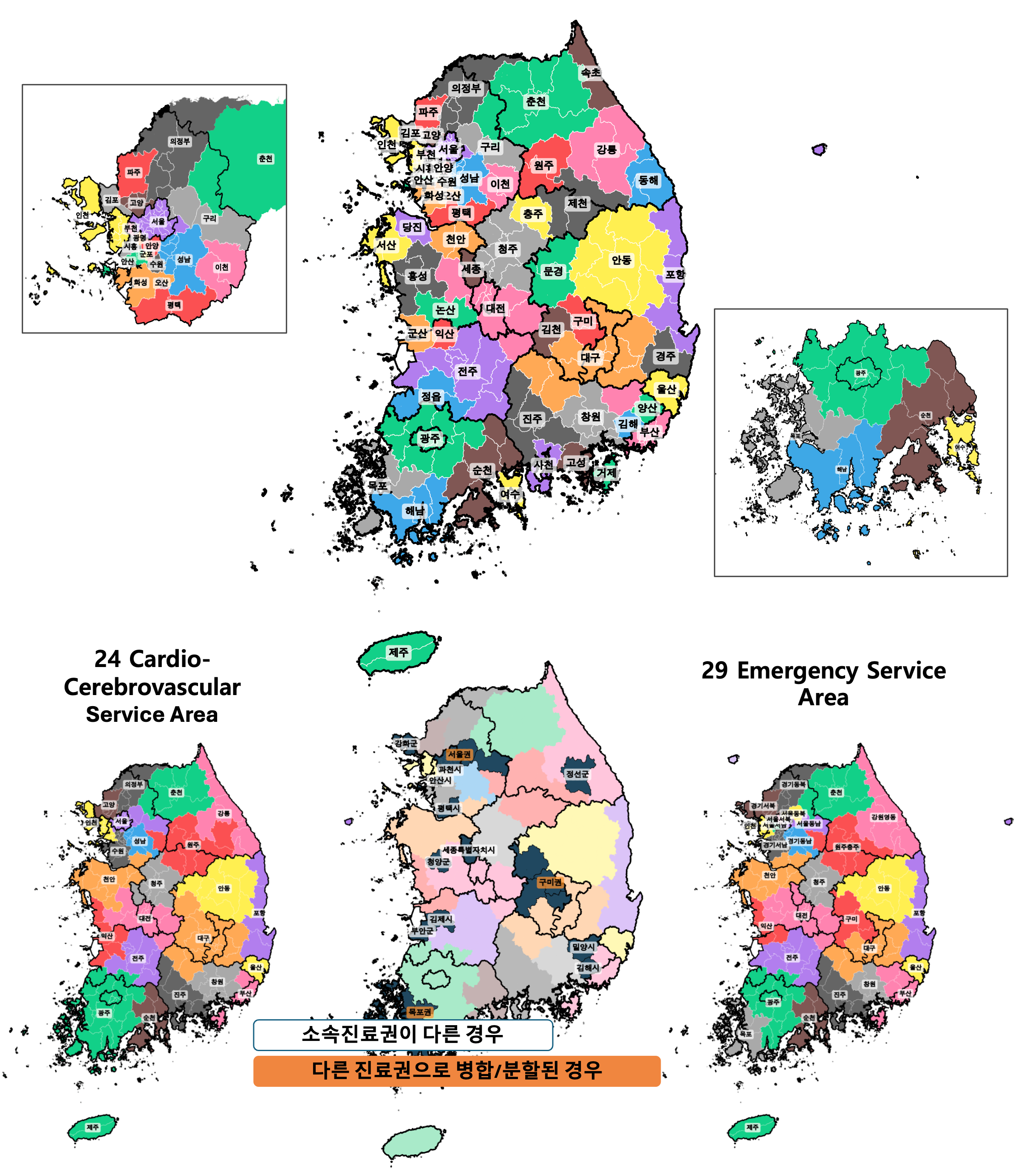
Delineation of Healthcare Service Area
This study aims to redefine Healthcare service areas for secondary and tertiary care in Korea to ensure equitable and effective healthcare distribution. Using the Relevance Index (RI) and Commitment Index (CI), the study evaluates and merges areas based on current medical utilization patterns. The need for this revision arises from significant changes in healthcare demands and demographic changes over the past decade, necessitating updates to the existing healthcare service areas. By modifying the Dartmouth Atlas delineation method and considering criteria like minimum population, self-sufficiency rates, and geographical proximity, the study proposes a revised framework of 60 healthcare service areas for secondary care. This new framework, based on recent data and accounting for the impact of COVID-19, aims to better reflect actual service usage and ensure efficient healthcare delivery across Korea.
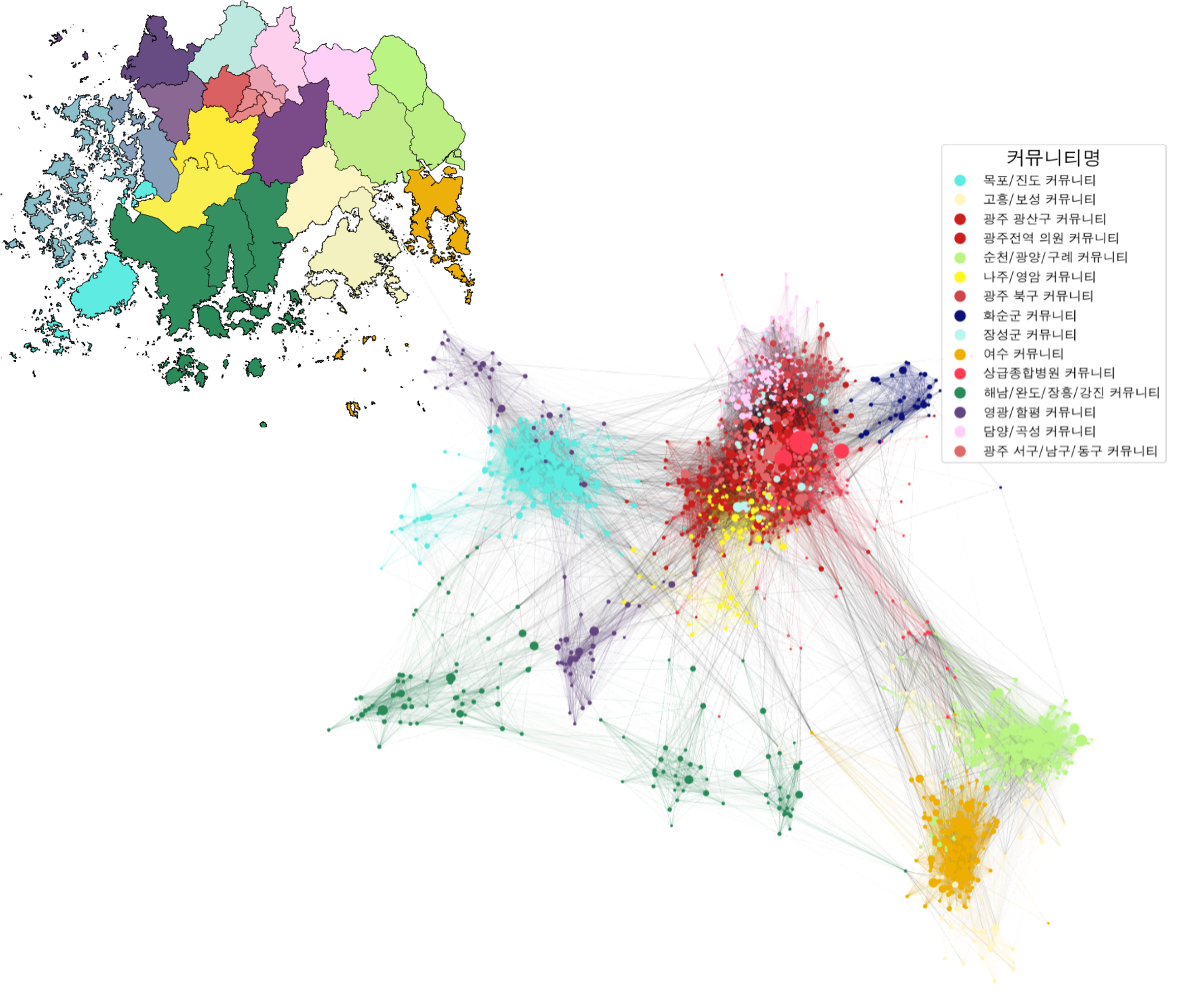
Analysis Framework for Patient Sharing Network
Healthcare system in Korea lacks an explicit patient referral and transfer procedure, highlighting the need for an establishment of a network-based cooperation system between healthcare institutions. This study proposes an analytical framework that extracts sequential medical usage events from NHIS claims data to construct a patient sharing network of healthcare institutions. By applying community detection algorithms to this network, we identify hospital clusters with high levels of cooperation and observe their geographical relationships and compositions. Ultimately, we analyze the relationships between institutions based on function and location, which serves as foundational knowledge for developing a hospital network system and an analytical tool to evaluate the results of policies and interventions.
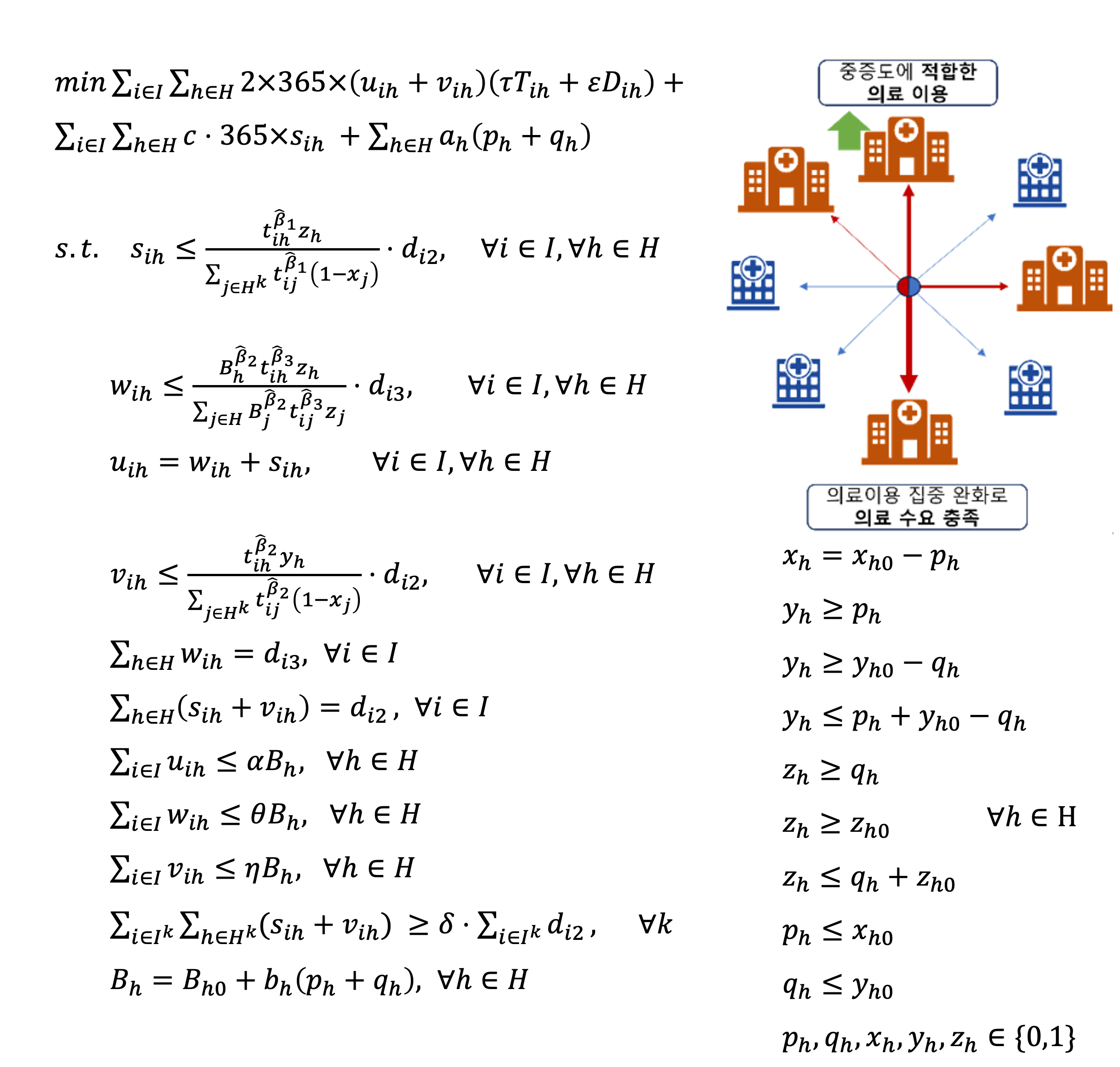
Optimization of Hospital Enhancement Decisions
This study addresses the necessity of redefining the healthcare supply structure in the Gwangju and Jeonnam regions. The analysis reveals that tertiary and secondary hospitals are under-supplied relative to demand, while regional and specialized hospitals are oversupplied. This imbalance results in patients frequently utilizing lower-tier hospitals than necessary, negatively impacting healthcare quality and outcomes. To address this, the study employs a mathematical optimization model to identify the optimal enhancement of existing hospitals' functions rather than establishing new ones. By strengthening secondary and regional hospitals, the healthcare delivery system can better meet demand and improve patient outcomes, ensuring higher quality care for all patients in the region.
